Delayed Hyper-Enhancement Magnetic Resonance Imaging Provides Incremental Diagnostic and Prognostic Utility in Suspected Cardiac Amyloidosis.
Bethany A. Austin, MD*, W.H. Wilson Tang, MD*, E. Rene Rodriguez, MD, Carmela Tan, MD, Scott D. Flamm, MD*,, David O. Taylor, MD*, Randall C. Starling, MD, MPH*, Milind Y. Desai, MD*.
Heart and Vascular Institute, Cleveland Clinic, Cleveland, Ohio Department of Pathology, Cleveland Clinic, Cleveland, Ohio Imaging Institute, Cleveland Clinic, Cleveland, Ohio.
Objectives: We sought to assess the diagnostic accuracy and incremental prognostic value of delayed hyper-enhancement cardiac magnetic resonance (DHE-CMR) compared with electrocardiographic and transthoracic echocardiographic (TTE) parameters in such patients.
Background: Utility of DHE-CMR in the diagnosis of patients with suspected cardiac amyloidosis (CA) has recently been demonstrated, but its incremental prognostic utility is unclear.
Methods: Forty-seven consecutive patients (mean age 63 years, 70% men, 55% New York Heart Association functional class >II) with suspected CA who underwent electrocardiography (ECG), TTE, DHE-CMR, and biopsy (38 endomyocardial, 9 extracardiac) were studied. Low voltage on ECG was defined as S-wave in lead V1 + R-wave in lead V5 or V6 <15 mm. TTE parameters, including deceleration time, E/E' ratio, and diastolic grade were recorded. CMR was considered positive with diffuse DHE of the subendocardium extending to adjacent myocardium. All-cause mortality was ascertained.
Results: In the study population, 59% had low voltage on ECG, 30% had abnormal deceleration time 150 ms, 38% had E/E' ratio >15, and 47% had advanced (pseudonormal or restrictive) diastology. The diagnostic accuracy of DHE-CMR in patients undergoing endomyocardial biopsy was as follows: sensitivity 88%, specificity 90%, positive predictive value 88%, and negative predictive value 90%. On multivariable logistic regression testing of the diagnostic ability of various noninvasive imaging parameters, only DHE-CMR was significant (Wald chi-square statistic 9.6, p < 0.01). At 1-year post-biopsy, there were 9 (19%) deaths. On Cox proportional hazards analysis, only positive DHE-CMR was a predictor of 1-year mortality (Wald chi-square statistic 4.91, p = 0.03).
Conclusions: A characteristic DHE-CMR pattern is more accurate for diagnosis and is a stronger predictor of 1-year mortality in patients with suspected CA as compared with other noninvasive parameters.
J Am Coll Cardiol Img, 2009; 2:1369-1377
Dec 30, 2009
Acute Myocardial Infarction: Serial Cardiac MR Imaging Shows a Decrease in Delayed Enhancement of the Myocardium during the 1st Week after Reperfusion1
Tareq Ibrahim, MD, Thomas Hackl, MD, Stephan G. Nekolla, PhD, Martin Breuer, MD, Michael Feldmair, MD, Albert Schömig, MD and Markus Schwaiger, MD
Purpose: To evaluate the time course of delayed gadolinium enhancement of infarcted myocardium by using serial contrast agent–enhanced (CE cardiac magnetic resonance (MR) images obtained during the acute, subacute, and chronic stages of infarction.
Materials and Methods: The study protocol was reviewed and approved by the local ethics committee, and written informed consent was obtained. Seventeen patients with reperfused acute myocardial infarction (AMI) underwent cine and CE cardiac MR a median of 1, 7, 35, and 180 days after reperfusion. Infarct size determined on the basis of delayed enhancement MR imaging at different times was compared by using nonparametric tests and Bland-Altman analysis. Extent of myocardial enhancement was compared with single photon emission computed tomographic (SPECT) measures of infarct size with Spearman correlation. Regional myocardial enhancement extent and contractility were analyzed with nonparametric tests.
Results: Infarct size was 18.3% of total myocardial LV volume on day 1 after AMI and decreased to 12.9% on day 7, 11.3% on day 35, and 11.6% on day 180 (all P < .001). Estimated infarct size on day 7, as compared with day 1 enhancement size, declined by 57.1% within the epicardium and by 6.3% within the endocardium (both P < .001). Infarct size on day 7 showed only minor changes at subsequent imaging and yielded a high correlation with SPECT measurements of infarct size (r = 0.84). Infarct size on day 7 inversely correlated with long-term wall thickening (P < .0001) and allowed prediction of contractile function.
Conclusion: In patients with AMI and successful coronary reperfusion, the size of delayed gadolinium enhancement at CE cardiac MR imaging significantly diminished during the 1st week after infarction. Thus, timing of CE cardiac MR imaging is crucial for accurate measurement of myocardial infarct size early after AMI.
Radiology January 2010 254:88-97.
Tareq Ibrahim, MD, Thomas Hackl, MD, Stephan G. Nekolla, PhD, Martin Breuer, MD, Michael Feldmair, MD, Albert Schömig, MD and Markus Schwaiger, MD
Purpose: To evaluate the time course of delayed gadolinium enhancement of infarcted myocardium by using serial contrast agent–enhanced (CE cardiac magnetic resonance (MR) images obtained during the acute, subacute, and chronic stages of infarction.
Materials and Methods: The study protocol was reviewed and approved by the local ethics committee, and written informed consent was obtained. Seventeen patients with reperfused acute myocardial infarction (AMI) underwent cine and CE cardiac MR a median of 1, 7, 35, and 180 days after reperfusion. Infarct size determined on the basis of delayed enhancement MR imaging at different times was compared by using nonparametric tests and Bland-Altman analysis. Extent of myocardial enhancement was compared with single photon emission computed tomographic (SPECT) measures of infarct size with Spearman correlation. Regional myocardial enhancement extent and contractility were analyzed with nonparametric tests.
Results: Infarct size was 18.3% of total myocardial LV volume on day 1 after AMI and decreased to 12.9% on day 7, 11.3% on day 35, and 11.6% on day 180 (all P < .001). Estimated infarct size on day 7, as compared with day 1 enhancement size, declined by 57.1% within the epicardium and by 6.3% within the endocardium (both P < .001). Infarct size on day 7 showed only minor changes at subsequent imaging and yielded a high correlation with SPECT measurements of infarct size (r = 0.84). Infarct size on day 7 inversely correlated with long-term wall thickening (P < .0001) and allowed prediction of contractile function.
Conclusion: In patients with AMI and successful coronary reperfusion, the size of delayed gadolinium enhancement at CE cardiac MR imaging significantly diminished during the 1st week after infarction. Thus, timing of CE cardiac MR imaging is crucial for accurate measurement of myocardial infarct size early after AMI.
Radiology January 2010 254:88-97.
Dec 28, 2009
Early Bird Registration for SCMR ends Dec 31!

Last days for early registration for the SCMR Thirteenth Annual Scientific Sessions
January 21-24, 2010:
http://www.scmr.org/meetings.html
Read the preliminary agenda: http://www.scmr.org/assets/files/meetings/SCMR_2010/Scientific%20Sessions%20Agenda.pdf
Tagging: review your knowledge

Both a powerful and under-utilized technique, myocardial tagging by CMR is reviewed in this open access JCMR paper by Shehata et al
http://jcmr-online.com/content/pdf/1532-429x-11-55.pdf
Juliano
Dec 22, 2009
Merry Christmas
Not everyday

Most of the responders do not perform CMR studies on a daily basis. Certainly this is a little disapointing but pushes us forward to augment the presence of the method in the daily cardiologic clinic. In my personal view, the exame is underutilized and still unknown to many cardiologists. Education, again, is the key here.
Dec 16, 2009
Brazilian paper on Circulation
A very interesting and comprehensive case report on Circulation by Loureiro et al.
Circulation. 2009;120:e285-e287
Juliano
Circulation. 2009;120:e285-e287
Juliano
Dec 13, 2009
FDA Paper on NSF
A very complete review on NSF by the FDA.
The PDF full text can be downloaded here (again, no virus or other unwanted stuff).
Juliano
The PDF full text can be downloaded here (again, no virus or other unwanted stuff).
Juliano
Early Bird Registration for SCMR ends Dec 31!

Registration for SCMR 2010 Meeting with lower prices ends on 2 weeks.
Hurry up to get the discounted rates!
http://www.scmr.org/meetings
Juliano
Dec 9, 2009
MR Angiography of Infrapopliteal Arteries in Patients with Peripheral Arterial Occlusive Disease by Using Gadofosveset at 3.0 T: Diagnostic Accuracy Compared with Selective DSA.
Harald Marcel Bonel, MD, Bettina Saar, MD, Hanno Hoppe, MD, Hak Hong Keo, MD, Marc Husmann, MD2, Konstantin Nikolaou, MD, Karin Ludwig, MD, Zsolt Szucs-Farkas, MD, PhD, Sudesh Srivastav, PhD and Ralph Kickuth, MD
Purpose: To prospectively compare the diagnostic accuracy of steady-state, high-spatial-resolution magnetic resonance (MR) angiography of the lower leg, performed with a blood pool contrast agent, with selective digital subtraction angiography (DSA) as the reference standard in patients with symptomatic peripheral arterial disease.
Materials and Methods: Local ethics committee approval and written informed consent were obtained. In a nonrandomized trial, selective DSA and MR angiography were performed at 3.0 T with a blood pool contrast agent on 22 calves in 20 patients (mean age, 69.4 years ± 11.3 [standard deviation]), 16 men (mean age, 67.8 years ± 12.4) and four women (mean age, 75.6 years ± 3.6 years), to evaluate 352 arterial segments. DSA and MR angiography were performed within 24 hours of each other and directly compared by three experienced, blinded radiologists by using high-spatial-resolution steady-state MR angiograms. Consensus reading for both DSA and MR angiography served as the reference standard.
Results: MR angiography was successful and occurred without serious adverse events in all patients. Seven significantly stenosed and 40 occluded segments were rated equally in both modalities. In three cases, the tibial arteries were shown to be occluded or significantly stenosed at DSA but appeared normal or significantly stenosed at MR angiography. The respective average segment sensitivity, specificity, and accuracy were 98.3% (59 of 60), 98% (113.7 of 116), and 98.1% (172.7 of 176) for DSA and 100% (60 of 60), 100% (116 of 116), and 100% (176 of 176) for MR angiography. Steady-state MR angiography was especially useful for the distal peroneal artery and the proximal anterior tibial artery.
Conclusion: MR angiography performed with blood pool agents has an accuracy comparable with that of selective DSA in the lower leg but with less risk involved. Steady-state imaging performed with blood pool agents facilitates evaluation of MR angiography of infrapopliteal arteries.
Radiology.December 2009; 253 (3)
Harald Marcel Bonel, MD, Bettina Saar, MD, Hanno Hoppe, MD, Hak Hong Keo, MD, Marc Husmann, MD2, Konstantin Nikolaou, MD, Karin Ludwig, MD, Zsolt Szucs-Farkas, MD, PhD, Sudesh Srivastav, PhD and Ralph Kickuth, MD
Purpose: To prospectively compare the diagnostic accuracy of steady-state, high-spatial-resolution magnetic resonance (MR) angiography of the lower leg, performed with a blood pool contrast agent, with selective digital subtraction angiography (DSA) as the reference standard in patients with symptomatic peripheral arterial disease.
Materials and Methods: Local ethics committee approval and written informed consent were obtained. In a nonrandomized trial, selective DSA and MR angiography were performed at 3.0 T with a blood pool contrast agent on 22 calves in 20 patients (mean age, 69.4 years ± 11.3 [standard deviation]), 16 men (mean age, 67.8 years ± 12.4) and four women (mean age, 75.6 years ± 3.6 years), to evaluate 352 arterial segments. DSA and MR angiography were performed within 24 hours of each other and directly compared by three experienced, blinded radiologists by using high-spatial-resolution steady-state MR angiograms. Consensus reading for both DSA and MR angiography served as the reference standard.
Results: MR angiography was successful and occurred without serious adverse events in all patients. Seven significantly stenosed and 40 occluded segments were rated equally in both modalities. In three cases, the tibial arteries were shown to be occluded or significantly stenosed at DSA but appeared normal or significantly stenosed at MR angiography. The respective average segment sensitivity, specificity, and accuracy were 98.3% (59 of 60), 98% (113.7 of 116), and 98.1% (172.7 of 176) for DSA and 100% (60 of 60), 100% (116 of 116), and 100% (176 of 176) for MR angiography. Steady-state MR angiography was especially useful for the distal peroneal artery and the proximal anterior tibial artery.
Conclusion: MR angiography performed with blood pool agents has an accuracy comparable with that of selective DSA in the lower leg but with less risk involved. Steady-state imaging performed with blood pool agents facilitates evaluation of MR angiography of infrapopliteal arteries.
Radiology.December 2009; 253 (3)
Noninvasive Assessment of Pulmonary Artery Flow and Resistance by Cardiac Magnetic Resonance in Congenital Heart Diseases With Unrestricted Left-to-Right.
Kings College London, BHF Centre of Excellence, Division of Imaging Sciences, London, United Kingdom Guy's and St. Thomas' NHS Foundation Trust Biomedical Research Centre, London, United Kingdom Division of Health and Social Care Research, Kings College, London, United Kingdom
Objectives: To determine whether noninvasive assessment of pulmonary artery flow (Qp) by cardiac magnetic resonance (CMR) would predict pulmonary vascular resistance (PVR) in patients with congenital heart disease characterized by an unrestricted left-to-right shunt.
Background: Patients with an unrestricted left-to-right shunt who are at risk of obstructive pulmonary vascular disease require PVR evaluation preoperatively. CMR cardiac catheter (XMR) combines noninvasive measurement of Qp by phase contrast imaging with invasive pressure measurement to accurately determine the PVR.
Methods: Patients referred for clinical assessment of the PVR were included. The XMR was used to determine the PVR. The noninvasive parameters, Qp and left-to-right shunt (Qp/Qs), were compared with the PVR using univariate regression models.
Results: The XMR was undertaken in 26 patients (median age 0.87 years)—ventricular septal defect 46.2%, atrioventricular septal defect 42.3%. Mean aortic flow was 2.24 ± 0.59 l/min/m2, and mean Qp was 6.25 ± 2.78 l/min/m2. Mean Qp/Qs was 2.77 ± 1.02. Mean pulmonary artery pressure was 34.8 ± 10.9 mm Hg. Mean/median PVR was 5.5/3.0 Woods Units (WU)/m2 (range 1.7 to 31.4 WU/m2). The PVR was related to both Qp and Qp/Qs in an inverse exponential fashion by the univariate regression equations PVR = exp(2.53 – 0.20[Qp]) and PVR = exp(2.75 – 0.52[Qp/Qs]). Receiver-operator characteristic (ROC) analysis was used to determine cutoff values for Qp and Qp/Qs above which the PVR could be regarded as clinically acceptable. A Qp of 6.05 l/min/m2 predicted a PVR of 3.5 WU/m2 with sensitivity 72%, specificity 100%, and area under the ROC curve 0.90 (p = 0.002). A Qp/Qs of 2.5/1 predicted a PVR of 3.5 WU/m2 with sensitivity 83%, specificity 100%, and area under the curve ROC 0.94 (p < 0.001).
Conclusions: Measurement of Qp or left-to-right shunt noninvasively by CMR has potential to predict the PVR in patients with an unrestricted left-to-right shunt and could potentially determine operability without having to undertake invasive testing.
Key Words: cardiac magnetic resonance • congenital • heart defects • pediatrics • pulmonary vascular resistance • shunts
J Am Coll Cardiol Img, 2009; 2:1285-1291.
Kings College London, BHF Centre of Excellence, Division of Imaging Sciences, London, United Kingdom Guy's and St. Thomas' NHS Foundation Trust Biomedical Research Centre, London, United Kingdom Division of Health and Social Care Research, Kings College, London, United Kingdom
Objectives: To determine whether noninvasive assessment of pulmonary artery flow (Qp) by cardiac magnetic resonance (CMR) would predict pulmonary vascular resistance (PVR) in patients with congenital heart disease characterized by an unrestricted left-to-right shunt.
Background: Patients with an unrestricted left-to-right shunt who are at risk of obstructive pulmonary vascular disease require PVR evaluation preoperatively. CMR cardiac catheter (XMR) combines noninvasive measurement of Qp by phase contrast imaging with invasive pressure measurement to accurately determine the PVR.
Methods: Patients referred for clinical assessment of the PVR were included. The XMR was used to determine the PVR. The noninvasive parameters, Qp and left-to-right shunt (Qp/Qs), were compared with the PVR using univariate regression models.
Results: The XMR was undertaken in 26 patients (median age 0.87 years)—ventricular septal defect 46.2%, atrioventricular septal defect 42.3%. Mean aortic flow was 2.24 ± 0.59 l/min/m2, and mean Qp was 6.25 ± 2.78 l/min/m2. Mean Qp/Qs was 2.77 ± 1.02. Mean pulmonary artery pressure was 34.8 ± 10.9 mm Hg. Mean/median PVR was 5.5/3.0 Woods Units (WU)/m2 (range 1.7 to 31.4 WU/m2). The PVR was related to both Qp and Qp/Qs in an inverse exponential fashion by the univariate regression equations PVR = exp(2.53 – 0.20[Qp]) and PVR = exp(2.75 – 0.52[Qp/Qs]). Receiver-operator characteristic (ROC) analysis was used to determine cutoff values for Qp and Qp/Qs above which the PVR could be regarded as clinically acceptable. A Qp of 6.05 l/min/m2 predicted a PVR of 3.5 WU/m2 with sensitivity 72%, specificity 100%, and area under the ROC curve 0.90 (p = 0.002). A Qp/Qs of 2.5/1 predicted a PVR of 3.5 WU/m2 with sensitivity 83%, specificity 100%, and area under the curve ROC 0.94 (p < 0.001).
Conclusions: Measurement of Qp or left-to-right shunt noninvasively by CMR has potential to predict the PVR in patients with an unrestricted left-to-right shunt and could potentially determine operability without having to undertake invasive testing.
Key Words: cardiac magnetic resonance • congenital • heart defects • pediatrics • pulmonary vascular resistance • shunts
J Am Coll Cardiol Img, 2009; 2:1285-1291.
Dec 6, 2009
Difficult exams in children
CMR in children is not so straightforward. This paper provides some hints on how to get better images when doing perfusion studies.
A direct link to the free PDF is here.
Research
Feasibility of perfusion cardiovascular magnetic resonance in paediatric patients
Emanuela R Valsangiacomo Buechel1 email, Christian Balmer1 email, Urs Bauersfeld1 email, Christian J Kellenberger2 email and Juerg Schwitter3 email
1University Children's Hospital Zurich, Division of Paediatric Cardiology, 8032 Zurich, Switzerland
2University Children's Hospital Zurich, Division of Diagnostic Imaging, 8032 Zurich, Switzerland
3University Hospital Zurich, Clinic of Cardiology, Zurich, Switzerland
author email corresponding author email
Journal of Cardiovascular Magnetic Resonance 2009, 11:51doi:10.1186/1532-429X-11-51
Published: 30 November 2009
Abstract
Aims
As coronary artery disease may also occur during childhood in some specific conditions, we sought to assess the feasibility and accuracy of perfusion cardiovascular magnetic resonance (CMR) in paediatric patients.
Methods and results
First-pass perfusion CMR studies were performed under pharmacological stress with adenosine and by using a hybrid echo-planar pulse sequence with slice-selective saturation recovery preparation. Fifty-six perfusion CMR examinations were performed in 47 patients. The median age was 12 years (1 month-18 years), and weight 42.8 kg (2.6-82 kg). General anaesthesia was required in 18 patients. Mean examination time was 67 ± 19 min. Diagnostic image quality was obtained in 54/56 examinations. In 23 cases the acquisition parameters were adapted to patient's size. Perfusion CMR was abnormal in 16 examinations. The perfusion defects affected the territory of the left anterior descending coronary artery in 11, of the right coronary artery in 3, and of the circumflex coronary artery in 2 cases. Compared to coronary angiography, perfusion CMR showed a sensitivity of 87% (CI 52-97%) and a specificity of 95% (CI 79-99%).
Conclusion
In children, perfusion CMR is feasible and accurate. In very young children (less than 1 year old), diagnostic image quality may be limited.
A direct link to the free PDF is here.
Research
Feasibility of perfusion cardiovascular magnetic resonance in paediatric patients
Emanuela R Valsangiacomo Buechel1 email, Christian Balmer1 email, Urs Bauersfeld1 email, Christian J Kellenberger2 email and Juerg Schwitter3 email
1University Children's Hospital Zurich, Division of Paediatric Cardiology, 8032 Zurich, Switzerland
2University Children's Hospital Zurich, Division of Diagnostic Imaging, 8032 Zurich, Switzerland
3University Hospital Zurich, Clinic of Cardiology, Zurich, Switzerland
author email corresponding author email
Journal of Cardiovascular Magnetic Resonance 2009, 11:51doi:10.1186/1532-429X-11-51
Published: 30 November 2009
Abstract
Aims
As coronary artery disease may also occur during childhood in some specific conditions, we sought to assess the feasibility and accuracy of perfusion cardiovascular magnetic resonance (CMR) in paediatric patients.
Methods and results
First-pass perfusion CMR studies were performed under pharmacological stress with adenosine and by using a hybrid echo-planar pulse sequence with slice-selective saturation recovery preparation. Fifty-six perfusion CMR examinations were performed in 47 patients. The median age was 12 years (1 month-18 years), and weight 42.8 kg (2.6-82 kg). General anaesthesia was required in 18 patients. Mean examination time was 67 ± 19 min. Diagnostic image quality was obtained in 54/56 examinations. In 23 cases the acquisition parameters were adapted to patient's size. Perfusion CMR was abnormal in 16 examinations. The perfusion defects affected the territory of the left anterior descending coronary artery in 11, of the right coronary artery in 3, and of the circumflex coronary artery in 2 cases. Compared to coronary angiography, perfusion CMR showed a sensitivity of 87% (CI 52-97%) and a specificity of 95% (CI 79-99%).
Conclusion
In children, perfusion CMR is feasible and accurate. In very young children (less than 1 year old), diagnostic image quality may be limited.
Dec 2, 2009
Wide and Three

The buzz at the RSNA 2009 on CMR was the use of the new hardware systems with 3T and wide 70cm bores from many vendors. This, combined with parallel imaging, seems to bring a new level of speed and temporal/spatial resolution to CMR exams. We still have to see the results of this on clinical papers as sites upgrade their machines to the newer platforms but the perspectives look very good (not cheap though!).
Nov 29, 2009
MVO as an endpoint

A couple of posts before we mentioned how CMR would become an important endpoint in clinical studies. This is another classical point in this regard. As soon as more sites prove their consistency in research, your cases/month can go up significantly. Participating in research always adds to your institution and generates more income.
J Am Coll Cardiol. 2009 Dec 1;54(23):2145-2153.
Impact of Primary Coronary Angioplasty Delay on Myocardial Salvage, Infarct Size, and Microvascular Damage in Patients With ST-Segment Elevation Myocardial Infarction Insight From Cardiovascular Magnetic Resonance.
Francone M, Bucciarelli-Ducci C, Carbone I, Canali E, Scardala R, Calabrese FA, Sardella G, Mancone M, Catalano C, Fedele F, Passariello R, Bogaert J, Agati L.
Cardiovascular Magnetic Resonance Unit, Department of Radiology Sciences, "Sapienza" University of Rome, Rome, Italy.
OBJECTIVES: We investigated the extent and nature of myocardial damage by using cardiovascular magnetic resonance (CMR) in relation to different time-to-reperfusion intervals. BACKGROUND: Previous studies evaluating the influence of time to reperfusion on infarct size (IS) and myocardial salvage in patients with ST-segment elevation myocardial infarction (STEMI) have yielded conflicting results. METHODS: Seventy patients with STEMI successfully treated with primary percutaneous coronary intervention within 12 h from symptom onset underwent CMR 3 +/- 2 days after hospital admission. Patients were subcategorized into 4 time-to-reperfusion (symptom onset to balloon) quartiles: 90 to 150 min (group II, n = 17), >150 to 360 min (group III, n = 17), and >360 min (group IV, n = 17). T2-weighted short tau inversion recovery and late gadolinium enhancement CMR were used to characterize reversible and irreversible myocardial injury (area at risk and IS, respectively); salvaged myocardium was defined as the normalized difference between extent of T2-weighted short tau inversion recovery and late gadolinium enhancement. RESULTS: Shorter time-to-reperfusion (group I) was associated with smaller IS and microvascular obstruction and larger salvaged myocardium. Mean IS progressively increased overtime: 8% (group I), 11.7% (group II), 12.7% (group III), and 17.9% (group IV), p = 0.017; similarly, MVO was larger in patients reperfused later (0.5%, 1.5%, 3.7%, and 6.6%, respectively, p = 0.047). Accordingly, salvaged myocardium markedly decreased when reperfusion occurred >90 min of coronary occlusion (8.5%, 3.2%, 2.4%, and 2.1%, respectively, p = 0.004). CONCLUSIONS: In patients with STEMI treated with primary percutaneous coronary intervention, time to reperfusion determines the extent of reversible and irreversible myocardial injury assessed by CMR. In particular, salvaged myocardium is markedly reduced when reperfusion occurs >90 min of coronary occlusion.
Too little, too far
Nov 23, 2009
Delayed enhancement in CMR: the "gold standard" for prognosis?

A couple of years ago many people debated whether CMR was the gold standard for viabiliby. Then came the gold standard for detection of infarcts. Are we into a new era as DLE stands for the gold standard of prognosis? In very wide and different scenarios DLE always seems to add prognostic information. This article by Dr. Cheong et al adds another point on the graph:
http://circ.ahajournals.org/cgi/content/abstract/120/21/2069?etoc
Prognostic Significance of Delayed-Enhancement Magnetic Resonance Imaging
Survival of 857 Patients With and Without Left Ventricular Dysfunction
Benjamin Y.C. Cheong, MD; Raja Muthupillai, PhD; James M. Wilson, MD; Angela Sung; Steffen Huber, MD; Samir Amin, BA; MacArthur A. Elayda, MD, PhD; Vei-Vei Lee, MS; Scott D. Flamm, MD
From the Departments of Radiology (B.Y.C.C., R.M., S.H., A.S., S.D.F.), Cardiology (B.Y.C.C., J.M.W., S.D.F.), and Biostatistics and Epidemiology (M.A.E., V.V.L.), the Texas Heart Institute at St. Luke’s Episcopal Hospital, and the Departments of Medicine (B.Y.C.C., S.A.) and Radiology (B.Y.C.C., R.M., S.D.F.), Baylor College of Medicine, Houston, Tex. Dr Flamm is currently at the Cleveland Clinic Foundation, Cleveland, Ohio.
Correspondence to B.Y.C. Cheong, MD, Department of Diagnostic and Interventional Radiology, St. Luke’s Episcopal Hospital and the Texas Heart Institute, 6720 Bertner Ave, MC 2–270, Houston, TX 77030. E-mail bcheong@sleh.com
Received January 20, 2009; accepted September 11, 2009.
Background— Left ventricular ejection fraction is a powerful independent predictor of survival in cardiac patients, especially those with coronary artery disease. Delayed-enhancement magnetic resonance imaging (DE-MRI) can accurately identify irreversible myocardial injury with high spatial and contrast resolution. To date, relatively limited data are available on the prognostic value of DE-MRI, so we sought to determine whether DE-MRI findings independently predict survival.
Methods and Results— The medical records of 857 consecutive patients who had complete cine and DE-MRI evaluation at a tertiary care center were reviewed regardless of whether the patients had coronary artery disease. The presence and extent of myocardial scar were evaluated qualitatively by a single experienced observer. The primary, composite end point was all-cause mortality or cardiac transplantation. Survival data were obtained from the Social Security Death Index. The median follow-up was 4.4 years; 252 patients (29%) reached one of the end points. Independent predictors of mortality or transplantation included congestive heart failure, ejection fraction, and age (P<0.0001 for each), as well as scar index (hazard ratio, 1.26; 95% confidence interval, 1.02 to 1.55; P=0.033). Similarly, in subsets of patients with or without coronary artery disease, scar index also independently predicted mortality or transplantation (hazard ratio, 1.33; 95% confidence interval, 1.05 to 1.68; P=0.018; and hazard ratio, 5.65; 95% confidence interval, 1.74 to 18.3; P=0.004, respectively). Cox regression analysis showed worse outcome in patients with any DE in addition to depressed left ventricular ejection fraction (<50%).
Conclusion— The degree of DE detected by DE-MRI appears to strongly predict all-cause mortality or cardiac transplantation after adjustment for traditional, well-known prognosticators.
Nov 22, 2009
Dyssynchrony analysis - a real niche for CMR

Dyssynchrony analysis is a new niche were CMR can provide a very comprehensive contribution by adding not only quantitative information but DLE visualization as well. The integration of data in this regard is a unique feature of CMR over all other methods. Paper pointed out by Dr. Florangel Martínez
Radiology. 2009 Nov;253(2):364-71. Epub 2009 Jul 31.
Interventricular mechanical dyssynchrony: quantification with velocity-encoded MR imaging.
Muellerleile K, Baholli L, Groth M, Barmeyer AA, Koopmann K, Ventura R, Koester R, Adam G, Willems S, Lund GK.
Center for Cardiology and Cardiovascular Surgery, University Medical Center Hamburg-Eppendorf, Martinistrasse 52, D-20246 Hamburg, Germany. ka.muellerleile@uke.de
PURPOSE: To evaluate the performance of velocity-encoded (VENC) magnetic resonance (MR) imaging, as compared with pulsed-wave echocardiography (PW-ECHO), in the quantification of interventricular mechanical dyssynchrony (IVMD) as a predictor of response to cardiac resynchronization therapy (CRT). MATERIALS AND METHODS: The study was approved by the local ethics committee, and all patients provided written informed consent. The study involved the examination of 45 patients (nine women, 36 men; median age, 60 years; interquartile age range, 47-69 years) with New York Heart Association class 2.0-3.0 heart failure and a reduced left ventricular ejection fraction (median, 25%; interquartile range, 21%-32%), with (n = 25) or without (n = 20) left bundle branch block. Aortic and pulmonary flow curves were constructed by using VENC MR imaging and PW-ECHO. IVMD was defined as the difference between the onset of aortic flow and the onset of pulmonary flow. Intraclass correlation coefficient, Spearman correlation coefficient, Bland-Altman, and Cohen kappa analyses were used to assess agreement between observers and methods. RESULTS: Inter- and intraobserver agreement regarding VENC MR imaging IVMD measurements was very good (intraclass r = 0.96, P < .001; mean bias, -3 msec +/- 11 [standard deviation] and 0 msec +/- 10, respectively). A strong correlation (Spearman r = 0.92, P < .001) and strong agreement (mean difference, -6 msec +/- 16) were found between VENC MR imaging and PW-ECHO in the quantification of IVMD. Agreement between VENC MR imaging and PW-ECHO in the identification of potential responders to CRT was excellent (Cohen kappa = 0.94). CONCLUSION: VENC MR measurements of IVMD are equivalent to PW-ECHO measurements and can be used to identify potential responders to CRT. (c) RSNA, 2009.
Nov 15, 2009
Cases Needed!

Submit your case to the Medis/SCMR SAT - DEADLINE Dec 1.
Need to be a SCMR member!
Juliano
>>>
Call for Cases: Medis/SCMR Self-Assessment Test 2010
Dear SCMR Member,
A popular and effective means of education, the Medis/SCMR Self-Assessment Test will be featured at the SCMR 2010 for the tenth consecutive year.
We are calling on you to share your interesting cardiac MR cases with other SCMR members through the Medis/SCMR Self-Assessment Test, so they too can learn from them.
The cases you provide will be peer-reviewed and you will be notified by e-mail if they are accepted. Cases used in the test at the SCMR 2010 will mention your name and affiliation.
Fast Online Submission of Cases
The online submission process consists of just five steps, allowing you to submit your cases in a few minutes' time.
1. Access the online Self-Assessment Center at http://scmr.medis.tv/
You can submit your cases using MS Internet Explorer version 6, 7 or 8.
2. If you are a first-time visitor, create your account and continue with submitting cases right away—no need to wait for your password.
3. Click 'Add new case' and provide a case description, a test question and three to six possible answers.
4. Add one to four images (JPG) or movies (AVI or MPG).
5. Preview and save your case.
You can add up to four cases. After you have submitted your cases, you can return to the online Self-Assessment Center any time to edit your cases, remove cases or to check their review status. You can access online help by clicking 'Manual' in the top right corner of the page.
Submission Deadline and More Info
Please submit your cases before December 1, to allow enough time for case review. If you have any questions or comments, please send an e-mail to info@medis.nl.
CMR Endpoints in Trials

Due to the accuracy and reduced variability, we should be seeing more and more in the use of CMR variables as endpoints in different trials. Of course the myocardium will always be a target but one cannot forget vascular wall assessment or functional data as well.
J Am Coll Cardiol. 2009 Nov 3;54(19):1787-94.
Effects of high-dose modified-release nicotinic acid on atherosclerosis and vascular function: a randomized, placebo-controlled, magnetic resonance imaging study.
Lee JM, Robson MD, Yu LM, Shirodaria CC, Cunnington C, Kylintireas I, Digby JE, Bannister T, Handa A, Wiesmann F, Durrington PN, Channon KM, Neubauer S, Choudhury RP.
Department of Cardiovascular Medicine, University of Oxford and Oxford Centre for Clinical Magnetic Resonance Research (OCMR), Oxford, United Kingdom.
Comment on:
* J Am Coll Cardiol. 2009 Nov 3;54(19):1795-6.
OBJECTIVES: Our aim was to determine the effects of high-dose (2 g) nicotinic acid (NA) on progression of atherosclerosis and measures of vascular function. BACKGROUND: NA raises high-density lipoprotein cholesterol (HDL-C) and reduces low-density lipoprotein cholesterol and is widely used as an adjunct to statin therapy in patients with coronary artery disease. Although changes in plasma lipoproteins suggest potential benefit, there is limited evidence of the effects of NA on disease progression when added to contemporary statin treatment. METHODS: We performed a double-blind, randomized, placebo-controlled study of 2 g daily modified-release NA added to statin therapy in 71 patients with low HDL-C (<40 mg/dl) and either: 1) type 2 diabetes with coronary heart disease; or 2) carotid/peripheral atherosclerosis. The primary end point was the change in carotid artery wall area, quantified by magnetic resonance imaging, after 1 year. RESULTS: NA increased HDL-C by 23% and decreased low-density lipoprotein cholesterol by 19%. At 12 months, NA significantly reduced carotid wall area compared with placebo (adjusted treatment difference: -1.64 mm(2) [95% confidence interval: -3.12 to -0.16]; p = 0.03). Mean change in carotid wall area was -1.1 +/- 2.6 mm(2) for NA versus +1.2 +/- 3.0 mm(2) for placebo. In both the treatment and placebo groups, larger plaques were more prone to changes in size (r = 0.4, p = 0.04 for placebo, and r = -0.5, p = 0.02 for NA). CONCLUSIONS: In statin-treated patients with low HDL-C, high-dose modified-release NA, compared with placebo, significantly reduces carotid atherosclerosis within 12 months. (Oxford Niaspan Study: Effects of Niaspan on Atherosclerosis and Endothelial Function; NCT00232531).
CMR conferences in Brazil

In 2010 we will have 6 big opportunities to meet and discuss CMR: 3 in the first semester and 3 in the second (dates to be announced soon). Interestingly, half organized by radiology and half by cardiologists, a definite plus in keeping both groups integrated. The focus of each meeting should be a little bit different, taking into account the public, the main objectives and the form of the meetings. Nevertheless, we believe the country has been very active and will continue to do so in the foreseeable future.
Nov 5, 2009
CMR and Angios go together
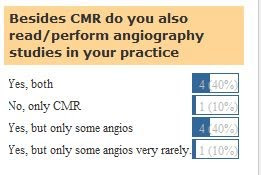
As a result of our poll, most CMR physicians perform both heart and angio studies. This is a very important issue since training in CMR has to take this point in consideration and make sure that fellows get enough exposure to the analysis of central and peripheral angio studies, enhancing their role as cardiovascular CMR imagers.
Nov 2, 2009
SCMR-LAC 2009 Annual Meeting

With the exceptional hospitality of Dr. Erick Alexanderson and all Mexican cardiologists, the SCMR-LAC 2009 Annual Meeting took place in Puebla, Nov 31. The meeting welcomed the presence of specialists from other areas with a very rich discussion on improvements in the chapter. Dr. Meave and Dr. Morelos as well as Dr. De LaPena inputs were very positive and we should provide a summary of the discussions very briefly in the site.
In the name of the chapter we openly thank the Mexican Society of Cardiology and Dr. Alexanderson for such a wonderful opportunity.
Oct 22, 2009
Feasibility of Cardiovascular Magnetic Resonance to Assess the Orifice Area of Aortic Bioprostheses
Florian von Knobelsdorff-Brenkenhoff, MD; André Rudolph, MD; Ralf Wassmuth, MD; Steffen Bohl, MD; Eva Elina Buschmann, MD; Hassan Abdel-Aty, MD; Rainer Dietz, MD and Jeanette Schulz-Menger, MD
From the Franz-Volhard-Klinik for Cardiology, HELIOS Klinikum Berlin Buch, University Medicine Berlin, Charité Campus Buch, Berlin, Germany.
Background— Prosthetic orifice area, usually calculated by transthoracic echocardiography (TTE) or transesophageal echocardiography (TEE), provides important information regarding the hemodynamic performance of aortic bioprostheses. However, both TTE and TEE have limitations; therefore accurate and reproducible determination of the orifice area often remains a challenge. The present study aimed to investigate the feasibility of cardiovascular magnetic resonance (CMR) to assess the orifice areas of aortic bioprostheses.
Methods and Results— CMR planimetry of the orifice area was performed in 65 patients (43/22 stented/stentless prostheses; mean time since implantation, 3.1±2.8 years; mean orifice area [TTE], 1.70±0.43 cm2; 62 normally functioning prostheses, 2 severe stenoses, and 1 severe regurgitation) in an imaging plane perpendicular to the transprosthetic flow using steady-state free-precession cine imaging under breath-hold conditions on a 1.5-T MR system. CMR results were compared with TTE (continuity equation, n=65) and TEE (planimetry, n=31). CMR planimetry was readily feasible in 80.0%; feasible with limitation in 15.4% because of stent, flow, and sternal wire artifacts; and impossible in 4.6% because of flow artifacts. Correlations of the orifice areas by CMR with TTE (r=0.82) and CMR with TEE (r=0.92) were significant. The average difference between the methods was –0.02±0.24 cm2 (TTE) and 0.05±0.15 cm2 (TEE). Agreement was present for stented and stentless devices and independent of orifice size. Intraobserver and interobserver variabilities of CMR planimetry were 6.7±5.4% and 11.5±7.8%.
Conclusions— The assessment of aortic bioprostheses with normal orifice areas by CMR is technically feasible and provides orifice areas with a close correlation to echocardiography and low observer dependency.
Key Words: imaging • MRI • echocardiography • valves • surgery
Circulation: Cardiovascular Imaging. 2009;2:397-404
Early Electrocardiographic Findings and MR Imaging-Verified Microvascular Injury and Myocardial Infarct Size
Robin Nijveldt, MD, PhD*,,*, Pieter A. van der Vleuten, MD, Alexander Hirsch, MD,, Aernout M. Beek, MD*, René A. Tio, MD, PhD, Jan G.P. Tijssen, PhD, Jan J. Piek, MD, PhD, Albert C. van Rossum, MD, PhD*,, Felix Zijlstra, MD, PhD
* Department of Cardiology, VU University Medical Center, Amsterdam, the NetherlandsInteruniversity Cardiology Institute of the Netherlands, Utrecht, the NetherlandsDepartment of Cardiology, University Medical Center Groningen, Groningen, the NetherlandsAcademic Medical Center, Amsterdam, the Netherlands
Objectives: This study investigated early electrocardiographic findings in relation to left ventricular (LV) function, extent and size of infarction, and microvascular injury in patients with acute myocardial infarction (MI) treated with percutaneous coronary intervention (PCI).
Background: The electrocardiogram (ECG) is the most used and simplest clinical method to evaluate the risk for patients immediately after reperfusion therapy for acute MI. ST-segment resolution and residual ST-segment elevation have been used for prognosis in acute MI, whereas Q waves are related to outcome in chronic MI. We hypothesized that the combination of these electrocardiographic measures early after primary PCI would enhance risk stratification.
Methods: We prospectively included 180 patients with a first acute ST-segment elevation MI to assess ST-segment resolution, residual ST-segment elevation, and number of Q waves using the 12-lead ECG acquired on admission and 1 h after successful PCI. The ECG findings were related to LV function, infarction size and transmurality, and microvascular injury as assessed with cine and gadolinium-enhanced cardiac magnetic resonance 4 ± 2 days after reperfusion therapy.
Results: Residual ST-segment elevation (β = –2.00, p = 0.004) and the number of Q waves (β = –1.66, p = 0.005) were independent ECG predictors of LV ejection fraction. Although the number of Q waves was the only independent predictor of infarct size (β = 2.01, p < 0.001) and transmural extent of infarction (β = 0.60, p < 0.001), residual ST-segment elevation was the only independent predictor of microvascular injury (odds ratio: 19.1, 95% confidence interval: 2.4 to 154, p = 0.005) in multivariable analyses. The ST-segment resolution was neither associated with LV function, infarct size, or transmurality indexes, nor with microvascular injury in multivariable analysis.
Conclusions: In patients after successful coronary intervention for acute MI, residual ST-segment elevation and the number of Q waves on the post-procedural ECG offer valuable complementary information on prediction of myocardial function and necrosis and its microvascular status.
Key Words: electrocardiography • cardiac magnetic resonance • myocardial infarction • left ventricular function
Am Coll Cardiol Img, 2009; 2:1187-1194.
Am Coll Cardiol Img, 2009; 2:1187-1194.
Oct 21, 2009
CMR for every patient with heart failure of unknown etiology?

The role of CMR in heart failure is elegantly reviewed in this manuscript in JACC:
The Role of Cardiovascular Magnetic Resonance Imaging in Heart Failure, Theodoros D. Karamitsos MD, PhDlow asterisk, Jane M. Francis DCC(R), DNMlow asterisk, Saul Myerson MDlow asterisk, Joseph B. Selvanayagam MBBS, DPhil† and Stefan Neubauer MD. Volume 54, Issue 15, 6 October 2009, Pages 1407-1424.
Now, should we use CMR in every patient with heart failure and dubious or unknown etiology? This is more controversial but the changes in management in those cases more than seem to justify this yet untested approach.
Oct 12, 2009
New SCMR-LAC Newsletter is out

Please download the PDF (118KB, virus-free double checked) at:
http://www.sendspace.com/file/4essdg
Juliano
CCT: Neutral/Positive for CMR


The results of the poll show a neutral/positive effect of CCT on CMR. In our case in Campinas, there was an increase in 20-30% in CMR after CCT. Not due to the fact that we have to check the functional aspects of lesions detected on CCT but to a general interest in advanced imaging as a whole. I still believe that both modalities help each other but the future will tell if that is really true.
CMR Reviews in Portuguese
From the Revista da SOCESP latest edition. The full PDF of the journal can be downloaded from:
http://www.socesp.org.br/revistasocesp/edicoes/volume19/pdf/v19_revista_n3.pdf
Juliano
http://www.socesp.org.br/revistasocesp/edicoes/volume19/pdf/v19_revista_n3.pdf
Juliano
Oct 11, 2009
Top Ten Articles in JCMR in 2009 - Free

Check out here: http://jcmr-online.com/mostviewedbyyear
Top 10 most accessed articles for last 30 days / past year / all time
1.
Accesses
3879 Review
Society for Cardiovascular Magnetic Resonance guidelines for reporting cardiovascular magnetic resonance examinations
W Gregory Hundley, David Bluemke, Jan G Bogaert, Matthias G Friedrich, Charles B Higgins, Mark A Lawson, Michael V McConnell, Subha V Raman, Albert C van Rossum, Scott Flamm, Christopher M Kramer, Eike Nagel, Stefan Neubauer
Journal of Cardiovascular Magnetic Resonance 2009, 11:5 (3 March 2009)
[Abstract] [Full Text] [PDF] [PubMed] [Related articles]
2.
Accesses
3656 Review
Role of cardiovascular magnetic resonance imaging in arrhythmogenic right ventricular dysplasia
Aditya Jain, Harikrishna Tandri, Hugh Calkins, David A Bluemke
Journal of Cardiovascular Magnetic Resonance 2008, 10:32 (20 June 2008)
[Abstract] [Full Text] [PDF] [PubMed] [Related articles]
3.
Accesses
3269 Review
Standardized cardiovascular magnetic resonance imaging (CMR) protocols, society for cardiovascular magnetic resonance: board of trustees task force on standardized protocols
Christopher M Kramer, Jorg Barkhausen, Scott D Flamm, Raymond J Kim, Eike Nagel
Journal of Cardiovascular Magnetic Resonance 2008, 10:35 (7 July 2008)
[Abstract] [Full Text] [PDF] [PubMed] [Related articles] [Cited on BioMed Central]
4.
Accesses
2837 Review
Cardiovascular magnetic resonance in pericardial diseases
Jan Bogaert, Marco Francone
Journal of Cardiovascular Magnetic Resonance 2009, 11:14 (4 May 2009)
[Abstract] [Full Text] [PDF] [PubMed] [Related articles] [Cited on BioMed Central]
5.
Accesses
2574 Review
Towards comprehensive assessment of mitral regurgitation using cardiovascular magnetic resonance
KM John Chan, Ricardo Wage, Karen Symmonds, Shelley Rahman-Haley, Raad H Mohiaddin, David N Firmin, John R Pepper, Dudley J Pennell, Philip J Kilner
Journal of Cardiovascular Magnetic Resonance 2008, 10:61 (22 December 2008)
[Abstract] [Full Text] [PDF] [PubMed] [Related articles] [Cited on BioMed Central]
6.
Accesses
2411 Review
Interventional cardiovascular magnetic resonance: still tantalizing
Kanishka Ratnayaka, Anthony Z Faranesh, Michael A Guttman, Ozgur Kocaturk, Christina E Saikus, Robert J Lederman
Journal of Cardiovascular Magnetic Resonance 2008, 10:62 (29 December 2008)
[Abstract] [Full Text] [PDF] [PubMed] [Related articles]
7.
Accesses
2322 Research
Normal values for aortic diameters in children and adolescents – assessment in vivo by contrast-enhanced CMR-angiography
Thomas Kaiser, Christian J Kellenberger, Manuela Albisetti, Eva Bergsträsser, Emanuela R Valsangiacomo Buechel
Journal of Cardiovascular Magnetic Resonance 2008, 10:56 (5 December 2008)
[Abstract] [Full Text] [PDF] [PubMed] [Related articles]
8.
Accesses
2305 Review
Myocardial first-pass perfusion cardiovascular magnetic resonance: history, theory, and current state of the art
Bernhard L Gerber, Subha V Raman, Krishna Nayak, Frederick H Epstein, Pedro Ferreira, Leon Axel, Dara L Kraitchman
Journal of Cardiovascular Magnetic Resonance 2008, 10:18 (28 April 2008)
[Abstract] [Full Text] [PDF] [PubMed] [Related articles] [Cited on BioMed Central]
9.
Accesses
2282 Research
Cardiovascular Magnetic Resonance and prognosis in cardiac amyloidosis
Alicia M Maceira, Sanjay K Prasad, Philip N Hawkins, Michael Roughton, Dudley J Pennell
Journal of Cardiovascular Magnetic Resonance 2008, 10:54 (25 November 2008)
[Abstract] [Full Text] [PDF] [PubMed] [Related articles] [Cited on BioMed Central]
10.
Accesses
2160 Research
Combined magnetic resonance coronary artery imaging, myocardial perfusion and late gadolinium enhancement in patients with suspected coronary artery disease
Christoph Klein, Rolf Gebker, Thomas Kokocinski, Stephan Dreysse, Bernhard Schnackenburg, Eckart Fleck, Eike Nagel
Journal of Cardiovascular Magnetic Resonance 2008, 10:45 (17 October 2008)
[Abstract] [Full Text] [PDF] [PubMed] [Related articles]
Oct 4, 2009
3rd SMCR-LAC Meeting

Don't miss: Puebla, Mexico. October 29 to November 2nd during the XXVI Congreso Nacional de Cardiologia de Mexico.
More information: http://www.congresocardiologia.org/start.asp
SCMR 2010 Regional Scholarship

US$1.500,00 + free registration to the meeting. ONE AWARD JUST FOR LATIN AMERICA as long as:
- you are a SCMR member
- you have an accepted oral or poster abstract for the meeting
Read the full information on
http://www.scmr.org/assets/files/meetings/SCMR_2010/SCMR%20Regional%20Scholarship%20Prog%20Description%20Website.pdf
There are no excuses not to apply!
Juliano
Sep 30, 2009
Prognostic value of adenosine stress cardiovascular magnetic resonance in patients with low-risk chest pain
Stamatios Lerakis , Dalton S McLean , Athanasios V Anadiotis , Matthew Janik , John N Oshinski , Nikolaos Alexopoulos , Elisa Zaragoza-Macias , Emir Veledar and Arthur E Stillman
Background
Approximately 5% of patients with an acute coronary syndrome are discharged from the emergency room with an erroneous diagnosis of non-cardiac chest pain. Highly accurate non-invasive stress imaging is valuable for assessment of low-risk chest pain patients to prevent these errors. Adenosine stress cardiovascular magnetic resonance (AS-CMR) is an imaging modality with increasing application. The goal of this study was to evaluate the negative prognostic value of AS-CMR among low-risk acute chest pain patients.
Methods
We studied 103 patients, mean 56.7+/-12.3 years of age, with chest pain and no electrocardiographic evidence of ischemia and negative cardiac biomarkers of necrosis, who were admitted to the Cardiac Decision Unit of our institution. All patients underwent AS-CMR. A negative AS-CMR was defined as absence of all the following: regional wall motion abnormalities at rest; perfusion defects during stress (adenosine) and rest; and myocardial scar on late gadolinium enhancement images. The patients were followed for a mean of 277 (range 161-462) days. The primary end point was defined as the combination of cardiac death, nonfatal acute myocardial infarction, re-hospitalization for chest pain, obstructive coronary artery disease (>50% coronary stenosis on invasive angiography) and coronary revascularization.
Approximately 5% of patients with an acute coronary syndrome are discharged from the emergency room with an erroneous diagnosis of non-cardiac chest pain. Highly accurate non-invasive stress imaging is valuable for assessment of low-risk chest pain patients to prevent these errors. Adenosine stress cardiovascular magnetic resonance (AS-CMR) is an imaging modality with increasing application. The goal of this study was to evaluate the negative prognostic value of AS-CMR among low-risk acute chest pain patients.
Methods
We studied 103 patients, mean 56.7+/-12.3 years of age, with chest pain and no electrocardiographic evidence of ischemia and negative cardiac biomarkers of necrosis, who were admitted to the Cardiac Decision Unit of our institution. All patients underwent AS-CMR. A negative AS-CMR was defined as absence of all the following: regional wall motion abnormalities at rest; perfusion defects during stress (adenosine) and rest; and myocardial scar on late gadolinium enhancement images. The patients were followed for a mean of 277 (range 161-462) days. The primary end point was defined as the combination of cardiac death, nonfatal acute myocardial infarction, re-hospitalization for chest pain, obstructive coronary artery disease (>50% coronary stenosis on invasive angiography) and coronary revascularization.
Results
In 14 patients (13.6%), AS-CMR was positive. The remaining 89 patients (86.4%), who had negative AS-CMR, were discharged. No patient with negative AS-CMR reached the primary end-point during follow-up. The negative predictive value of AS-CMR was 100%.
In 14 patients (13.6%), AS-CMR was positive. The remaining 89 patients (86.4%), who had negative AS-CMR, were discharged. No patient with negative AS-CMR reached the primary end-point during follow-up. The negative predictive value of AS-CMR was 100%.
Conclusions
AS-CMR holds promise as a useful tool to rule out significant coronary artery disease in patients with low-risk chest pain. Patients with negative AS-CMR have an excellent short and mid-term prognosis.
AS-CMR holds promise as a useful tool to rule out significant coronary artery disease in patients with low-risk chest pain. Patients with negative AS-CMR have an excellent short and mid-term prognosis.
Journal of Cardiovascular Magnetic Resonance 2009, 11:37.
Sep 21, 2009
Magnetic resonance investigations in Brugada syndrome reveal unexpectedly high rate of structural abnormalities
Oronzo Catalano,*, Serena Antonaci, Guido Moro, Maria Mussida1, Mauro Frascaroli, Maurizia Baldi2, Franco Cobelli, Paola Baiardi, Janni Nastoli, Raffaella Bloise, Nicola Monteforte, Carlo Napolitano and Silvia G. Priori.
Aims: Recent data suggest that sub-clinical structural abnormalities may be part of the Brugada syndrome (BrS) phenotype, a disease traditionally thought to occur in the structurally normal heart. In this study, we carried out detailed assessment of cardiac morphology and function using cardiac magnetic resonance imaging (CMRI).
Methods and results: Thirty consecutive patients with BrS were compared with 30 sex- (26/4 male/female), body surface area- (±0.2 m2), and age-matched (±5 years) normal volunteers. CMRI exam included long- and short-axis ECG-gated breath-hold morphological T1-TSE sequences for fatty infiltration and cine-SSFP sequences for kinetic assessment. Fatty infiltration was not found in any subject. Patients with BrS compared with normal subjects showed higher incidence of mild right ventricle (RV) wall-motion abnormalities [15 (50%) vs. 5 (17%) subjects (P = 0.006) with reduced radial fractional shortening in more than two segments], reduction of outflow tract ejection fraction (49 ± 11% vs. 55 ± 10%; P = 0.032), enlargement of the inflow tract diameter (46 ± 4 vs. 41 ± 5 mm, P < 0.001 in short-axis; 46 ± 4 vs. 42 ± 5 mm, P = 0.001 in four-chamber long-axis view) and area (22 ± 2 vs. 20 ± 3 cm2; P = 0.050), and of global RV end-systolic volume (34 ± 10 vs. 30 ± 6 mL/m2; P = 0.031) but comparable outflow tract dimensions, global RV end-diastolic volume, left ventricle parameters, and atria areas.
Conclusion: CMRI detects a high prevalence of mild structural changes of the RV, and suggests further pathophysiological complexity in BrS. Prospective studies to assess the long-term evolution of such abnormalities are warranted.
Key Words: Brugada syndrome • Cardiac magnetic resonance imaging • Sudden cardiac death • SCN5A.
European Heart Journal 2009 30(18):2241-2248
Prediction of All-Cause Mortality From Global Longitudinal Speckle Strain
Comparison With Ejection Fraction and Wall Motion Scoring
Comparison With Ejection Fraction and Wall Motion Scoring
Tony Stanton, MBChB, PhD; Rodel Leano, BS and Thomas H. Marwick, MBBS, PhD
From the School of Medicine, University of Queensland, Brisbane, Australia.
From the School of Medicine, University of Queensland, Brisbane, Australia.
Background— Although global left ventricular systolic function is an important determinant of mortality, standard measures such as ejection fraction (EF) and wall motion score index (WMSI) have important technical limitations. The aim of this study was to compare global longitudinal speckle strain (GLS), an automated technique for measurement of long-axis function, with EF and WMSI for the prediction of mortality.
Methods and Results— Of 546 consecutive individuals undergoing echocardiography for assessment of resting left ventricular function, 91 died over a period of 5.2±1.5 years. In addition to Simpson biplane EF, WMSI was determined by 2 experienced readers and GLS was calculated from 3 standard apical views using 2D speckle tracking. The incremental value of EF, WMSI, and GLS to significant clinical variables was assessed in nested Cox models. Clinical factors associated with outcome (model 2=20.2) were age (hazard ratio [HR], 1.46; P<0.01), p="0.01)," p="0.03)" 2="34.9,">35% and those with and without wall motion abnormalities. A GLS –12% was found to be equivalent to an EF 35% for the prediction of prognosis. Intraobserver and interobserver variations for EF and GLS were similar.
Conclusions— GLS is a superior predictor of outcome to either EF or WMSI and may become the optimal method for assessment of global left ventricular systolic function.
Key Words: echocardiography • ventricular function • strain • mortality
Circ Cardiovasc Imaging.2009; 2: 353-355 .
Accuracy of Cardiac Magnetic Resonance of Absolute Myocardial Blood Flow With a High-Field System
Comparison With Conventional Field Strength
Comparison With Conventional Field Strength
Timothy F. Christian, MD*,*, Stephen P. Bell, BS*, Lawrence Whitesell, BS, Michael Jerosch-Herold, PhD
Objectives: The aim of this study was to determine the accuracy of cardiac magnetic resonance (CMR) first pass (FP) perfusion measures of absolute myocardial blood flow (MBF) with a 3.0-T magnet and compare these measures with FP perfusion at 1.5-T with absolute MBF by labeled microspheres as the gold standard.
Background: First-pass magnetic resonance (MR) myocardial perfusion imaging can quantify MBF, but images are of low signal at conventional magnetic field strength due to the need for rapid acquisition.
Background: First-pass magnetic resonance (MR) myocardial perfusion imaging can quantify MBF, but images are of low signal at conventional magnetic field strength due to the need for rapid acquisition.
Methods: A pig model was used to alter MBF in a coronary artery during FP CMR (intracoronary adenosine followed by ischemia). This produces an active zone with a range of MBF and a control zone. Microspheres were injected into the left atrium with concurrent reference sampling. FP MR perfusion imaging was performed at 1.5-T (n = 9) or 3.0-T (n = 8) with a saturation-recovery gradient echo sequence in short-axis slices during a bolus injection of 0.025 mmol/kg gadolinium–diethylenetriamine pentaacetic acid. Fermi function deconvolution was performed on active and control region of interest from short-axis slices with an arterial input function derived from the left ventricular cavity. These MR values of MBF were matched to microsphere values obtained from short-axis slices at pathology.
Results: Occlusion MBF was 0.21 ± 0.26 ml/min/g, adenosine MBF was 2.28 ± 0.99 ml/min/g, and control zone MBF was 0.70 ± 0.22 ml/min/g. The correlation of MR FP CMR with microsphere was close for both field strengths: 3.0-T, r = 0.98, p < 0.0001 and 1.5-T, r = 0.95, p < 0.0001. The 95% confidence limits of agreement were slightly narrower at 3.0-T (3.0-T = 0.49 ml/min/g, 1.5-T = 0.68 ml/min/g, p < 0.05). The FP CMR image characteristics were better at 3.0-T (noise and contrast enhancement were both superior at 3.0-T). In myocardial zones where MBF <0.50 ml/min/g, the correlation with microspheres was closer at 3.0-T (r = 0.55 at 1.5-T, r = 0.85 at 3.0-T).
Conclusions: Absolute MBF by FP perfusion imaging is accurate at both 1.5- and 3.0-T. Signal quality is better at 3.0-T, which might confer a benefit for estimating MBF in ischemic zones.
Key Words: cardiac imaging • CMR • coronary flow reserve • ischemia • myocardial perfusion
J Am Coll Cardiol Img, 2009; 2:1103-1110.
Sep 20, 2009
Will you care for a free Windows CMR Software?


For those of us who need a good CMR software for non commercial uses, a nice pick is Segment. It provides most of the features found in full fledged commercial packages and is upgraded many times a year. Thanks to Einar Heiberg at the Cardiac MR group, at Lund University, Sweden.
http://segment.heiberg.se/index.htm
Sep 17, 2009
Regadenason review

I have followed the work on this new agent in the last few years. I tried to test it in CMR perfusion but the company refused it initially. It was only tested with nuclear MPI. On a critical view: the symptoms are about the same as adenosine (ok, there is a statistical difference but I believe clinically irrelevant) but the ease of use really is something to cheer. It would fit CMR very nicely: one single bolus, no weight ajustement, short duration in minutes.
However, as it is, the price is almost prohibitive and it is not approved in all countries yet (at least not in Brazil so far).
If the prices go down (and there are 2 competitors coming along), maybe it will be useful. Otherwise, good old dipyridamole will continue ruling.
What a difference by what was reported in JACC
Braziliam team looks at MDE in PH
A very well written article by a Brazilian team. Congratulations!
Br J Radiol. 2009 Apr 27. [Epub ahead of print]
Myocardial delayed enhancement in patients with pulmonary hypertension and right ventricular failure: evaluation by cardiac MRI.
Junqueira FP, Filho RM, Coutinho AC, Loureiro R, DE Pontes PV, Domingues RC, Dro Gasparetto EL.
Clinics Multi-Imagem, 2Clínica de Diagnóstico Por Imagem and 3Department of Radiology, University of Rio de Janeiro, Rio de Janeiro, Brazil.
In this study we evaluated patients with pulmonary arterial hypertension (PAH) and impaired right ventricular function. We used cardiac MRI for the detection of myocardial delayed enhancement (MDE) and its possible association with other clinical variables. 20 patients (6 males and 14 females, aged 44.5+/-11 years; 15 New York Heart Association class III, 5 class IV) with known PAH (13 idiopathic, 7 resulting from chronic pulmonary embolism) were evaluated for the detection of MDE. Short-axis cine images of the heart were made for ventricular function assessment using a steady-state free precession sequence. For MDE evaluation, a short-axis phase-sensitive inversion recovery sequence was performed 10 min after intravenous administration of 0.2 mmol kg(-1) gadodiamide. Right ventricle (RV) systolic dysfunction, RV enlargement and RV hypertrophy were present in 20 patients (RV ejection fraction, 21.5+/-7.2 %; RV diastolic diameter, 5.97+/-0.79 cm; RV wall thickness, 0.73+/-0.10 cm). 13 of the 20 patients (65%) were positive for MDE (10 anterior, 12 inferior). All 13 positive patients with MDE demonstrated small hyperintense areas at the insertion points of the RV free wall in the interventricular septum. We found no significant correlation between MDE and ejection fraction or other haemodynamic variables. In this study MDE correlated positively only with the duration of disease. We found that septal MDE can be present in patients with PAH and impaired ventricular function. However, further studies are necessary to investigate this possible association and its prognostic implication.
Br J Radiol. 2009 Apr 27. [Epub ahead of print]
Myocardial delayed enhancement in patients with pulmonary hypertension and right ventricular failure: evaluation by cardiac MRI.
Junqueira FP, Filho RM, Coutinho AC, Loureiro R, DE Pontes PV, Domingues RC, Dro Gasparetto EL.
Clinics Multi-Imagem, 2Clínica de Diagnóstico Por Imagem and 3Department of Radiology, University of Rio de Janeiro, Rio de Janeiro, Brazil.
In this study we evaluated patients with pulmonary arterial hypertension (PAH) and impaired right ventricular function. We used cardiac MRI for the detection of myocardial delayed enhancement (MDE) and its possible association with other clinical variables. 20 patients (6 males and 14 females, aged 44.5+/-11 years; 15 New York Heart Association class III, 5 class IV) with known PAH (13 idiopathic, 7 resulting from chronic pulmonary embolism) were evaluated for the detection of MDE. Short-axis cine images of the heart were made for ventricular function assessment using a steady-state free precession sequence. For MDE evaluation, a short-axis phase-sensitive inversion recovery sequence was performed 10 min after intravenous administration of 0.2 mmol kg(-1) gadodiamide. Right ventricle (RV) systolic dysfunction, RV enlargement and RV hypertrophy were present in 20 patients (RV ejection fraction, 21.5+/-7.2 %; RV diastolic diameter, 5.97+/-0.79 cm; RV wall thickness, 0.73+/-0.10 cm). 13 of the 20 patients (65%) were positive for MDE (10 anterior, 12 inferior). All 13 positive patients with MDE demonstrated small hyperintense areas at the insertion points of the RV free wall in the interventricular septum. We found no significant correlation between MDE and ejection fraction or other haemodynamic variables. In this study MDE correlated positively only with the duration of disease. We found that septal MDE can be present in patients with PAH and impaired ventricular function. However, further studies are necessary to investigate this possible association and its prognostic implication.
Sep 8, 2009
A trial to watch for

This will answer very important questions partially responded by MR-Impact. Let's eagerly wait for its results.
Trials. 2009 Jul 29;10:62.Click here to read Links
Clinical evaluation of magnetic resonance imaging in coronary heart disease: the CE-MARC study.
Greenwood JP, Maredia N, Radjenovic A, Brown JM, Nixon J, Farrin AJ, Dickinson C, Younger JF, Ridgway JP, Sculpher M, Ball SG, Plein S.
Division of Cardiovascular and Neuronal Remodelling, Leeds Institute of Genetics, Health and Therapeutics, University of Leeds, Leeds General Infirmary, Leeds, LS1 3EX, UK. j.greenwood@leeds.ac.uk
BACKGROUND: Several investigations are currently available to establish the diagnosis of coronary heart disease (CHD). Of these, cardiovascular magnetic resonance (CMR) offers the greatest information from a single test, allowing the assessment of myocardial function, perfusion, viability and coronary artery anatomy. However, data from large scale studies that prospectively evaluate the diagnostic accuracy of multi-parametric CMR for the detection of CHD in unselected populations are lacking, and there are few data on the performance of CMR compared with current diagnostic tests, its prognostic value and cost-effectiveness. METHODS/DESIGN: This is a prospective diagnostic accuracy cohort study of 750 patients referred to a cardiologist with suspected CHD. Exercise tolerance testing (ETT) will be preformed if patients are physically able. Recruited patients will then undergo CMR and single photon emission tomography (SPECT) followed in all patients by invasive X-ray coronary angiography. The order of the CMR and SPECT tests will be randomised. The CMR study will comprise rest and adenosine stress perfusion, cine imaging, late gadolinium enhancement and whole-heart MR coronary angiography. SPECT will use a gated stress/rest protocol. The primary objective of the study is to determine the diagnostic accuracy of CMR in detecting significant coronary stenosis, as defined by X-ray coronary angiography. Secondary objectives include an assessment of the prognostic value of CMR imaging, a comparison of its diagnostic accuracy against SPECT and ETT, and an assessment of cost-effectiveness. DISCUSSION: The CE-MARC study is a prospective, diagnostic accuracy cohort study of 750 patients assessing the performance of a multi-parametric CMR study in detecting CHD using invasive X-ray coronary angiography as the reference standard and comparing it with ETT and SPECT. TRIAL REGISTRATION: Current Controlled Trials ISRCTN77246133.
Sep 7, 2009
Location of LGE gives more information on non-ischaemic dilated cardiomyopathy
A difference between mid and epicardial LGE was found giving more prognostic information in non-ischaemic dilated cardiomyopathy.
Eur J Heart Fail. 2009 Jun;11(6):573-80. Epub 2009 Apr 21.
Patterns of late gadolinium enhancement are associated with ventricular stiffness in patients with advanced non-ischaemic dilated cardiomyopathy.
Choi EY, Choi BW, Kim SA, Rhee SJ, Shim CY, Kim YJ, Kang SM, Ha JW, Chung N.
Cardiology Division, Yonsei Cardiovascular Center and Cardiovascular Research Institute, Shinchon-dong 134, Seoul, South Korea 120-752.
AIMS: Despite the prognostic importance of ventricular filling and ventricular-arterial interaction in patients with advanced systolic heart failure, the structural determinants of these parameters have not been fully studied. We aimed to investigate whether patterns of late gadolinium enhancement (LGE) on cardiac magnetic resonance affect ventricular elastic properties or performance in patients with non-ischaemic dilated cardiomyopathy (DCM). METHODS AND RESULTS: Patients (n = 49) with markedly reduced systolic function (left ventricular (LV) ejection fraction <35%) due to longstanding non-ischaemic DCM underwent contrast-enhanced cardiac magnetic resonance after comprehensive echo-Doppler evaluations. The single beat-derived end-diastolic elastance, end-systolic elastance, arterial elastance, and dyssynchrony indices were measured by echo. On the basis of LGE patterns, patients could be divided into three groups: non-LGE (n = 18), non-midwall LGE (n = 13), and midwall LGE (n = 18). The midwall LGE group had lower LV systolic longitudinal velocity (4.6 +/- 1.7 for non-LGE vs. 4.3 +/- 1.2 for non-midwall LGE vs. 3.5 +/- 1.0 cm/s for midwall LGE, P = 0.025), higher end-diastolic elastance index (0.41 +/- 0.21 vs. 0.46 +/- 0.31 vs. 0.85 +/- 0.51 respectively, P = 0.008), and a more impaired ventriculoarterial coupling index (3.14 +/- 1.53 vs. 2.88 +/- 1.94 vs. 5.52 +/- 3.18, P = 0.006) than other subgroups. CONCLUSION: Patients with midwall LGE had a higher ventricular stiffness index and more impaired ventriculoarterial coupling when compared with other non-ischaemic DCM patients.
Eur J Heart Fail. 2009 Jun;11(6):573-80. Epub 2009 Apr 21.
Patterns of late gadolinium enhancement are associated with ventricular stiffness in patients with advanced non-ischaemic dilated cardiomyopathy.
Choi EY, Choi BW, Kim SA, Rhee SJ, Shim CY, Kim YJ, Kang SM, Ha JW, Chung N.
Cardiology Division, Yonsei Cardiovascular Center and Cardiovascular Research Institute, Shinchon-dong 134, Seoul, South Korea 120-752.
AIMS: Despite the prognostic importance of ventricular filling and ventricular-arterial interaction in patients with advanced systolic heart failure, the structural determinants of these parameters have not been fully studied. We aimed to investigate whether patterns of late gadolinium enhancement (LGE) on cardiac magnetic resonance affect ventricular elastic properties or performance in patients with non-ischaemic dilated cardiomyopathy (DCM). METHODS AND RESULTS: Patients (n = 49) with markedly reduced systolic function (left ventricular (LV) ejection fraction <35%) due to longstanding non-ischaemic DCM underwent contrast-enhanced cardiac magnetic resonance after comprehensive echo-Doppler evaluations. The single beat-derived end-diastolic elastance, end-systolic elastance, arterial elastance, and dyssynchrony indices were measured by echo. On the basis of LGE patterns, patients could be divided into three groups: non-LGE (n = 18), non-midwall LGE (n = 13), and midwall LGE (n = 18). The midwall LGE group had lower LV systolic longitudinal velocity (4.6 +/- 1.7 for non-LGE vs. 4.3 +/- 1.2 for non-midwall LGE vs. 3.5 +/- 1.0 cm/s for midwall LGE, P = 0.025), higher end-diastolic elastance index (0.41 +/- 0.21 vs. 0.46 +/- 0.31 vs. 0.85 +/- 0.51 respectively, P = 0.008), and a more impaired ventriculoarterial coupling index (3.14 +/- 1.53 vs. 2.88 +/- 1.94 vs. 5.52 +/- 3.18, P = 0.006) than other subgroups. CONCLUSION: Patients with midwall LGE had a higher ventricular stiffness index and more impaired ventriculoarterial coupling when compared with other non-ischaemic DCM patients.
Sep 2, 2009
The Value of Cardiac Magnetic Resonance in
Patients With Acute Coronary Syndrome and
Normal Coronary Arteries
Introduction and objectives. A number of different conditions can present with symptoms similar to acute coronary syndrome (ACS): chest pain, electrocardiographic changes and elevated levels of markers of myocardial damage. Even after coronary angiography has been performed, differential diagnosis can be challenging. The aim of this study was to evaluate the usefulness of cardiacmagnetic resonance (CMR) for diagnosing conditions that present like ACS but in which the coronary arteries are normal.
Methods. The study involved 80 patients with suspected ACS and normal coronary arteries. Their mean age was 48±15 years and their mean troponin-T (TnT) level was 1.8±0.9 ng/ml. A CMR study, which involved T2- weighted imaging to detect edema and delayed contrastenhancement (DCE) imaging 10 minutes after gadolinium administration, was performed.
Results. In 51 patients (63%), the final diagnosis was acute myocarditis. In all these cases, DCE was observed in subepicardial and middle segments of the myocardium. The final diagnosis was acute myocardial infarction in 12 patients (15%), all of whom exhibited subendocardial or transmural DCE. In the 9 (11%) who exhibited abnormal contractility on baseline echocardiography with subsequent normalization, CMR did not show DCE, a finding that is characteristic of Takotsubo cardiomyopathy. In addition, 4 patients had a final diagnosis of pericarditis, while no diagnosis could be established in another 4.
Conclusions. The clinical presentation of acute myocarditis and Takotsubo syndrome can be similar to that of ACS. The presence and distribution of DCE on CMR are of great help in establishing a diagnosis.
Key words: Cardiac magnetic resonance. Myocarditis. Acute coronary syndrome. Takotsubo.
Rev Esp Cardiol. 2009;62(9):976-83
Sep 1, 2009
Congreso virtual de Cardiología!!!
"Estimados amigos del foro, los invito a participar del 6to Congreso Virtual de Cardiología de la Federación Argentina de Cardiología (FAC). Es totalmente gratuito. Pueden enviar trabajos o particiar en las mesas de discusión con panelistas de primer nuvel internacional."
VI Congreso Internacional de Cardiología por Internet
1ro. de Septiembre al 30 de Noviembre de 2009
Declarado de Interés Nacional
Res. Nº Res. Nº 363 - 361 - 04/2009
Presidencia de la Nación - Ministerio de Salud de la Nación Argentina.
Comienza hoy..
www.fac.org.ar/6cvc
Si aún no lo ha hecho, lo invitamos a inscribirse y a interactuar con los conferencistas y autores a través de los Foros de Discusión, donde los mensajes contarán con traducción.
Principales temas que se abordarán:
Cardiopatía Isquémica – RCP – Síndrome Metabólico – Dislipemias – Insuficiencia Cardíaca – Arritmias – Dispositivos electrónicos para el tratamiento de trastornos de la conducción – Enfermedad de Chagas – Hipertrofia ventricular – Investigación Clínica – HTA – Cirugía de revascularización – Angioplastia – Prótesis Endoluminales
Speakers internacionales que participarán en esta edición:
Dr. Paul A. Levine (EEUU); Dr. Adrian Baranchuk (EEUU); Dr. Andrés Ricardo Pérez Riera (Brasil); Dr. Jose Carlos Pachon (Brasil); Dr. Juan Carlos Chachques (Francia); Dr. Josep Brugada (España); Dr. Robert M. Lang (EEUU); Dr. Arturo Evangelista (España); Dr. Wilson Mathias (Brasil); Dr. James K. McCord (EEUU); Dr. Xavier Bosch (España); Dr. Michael A. Ross (EEUU); Dr. Juan José Badimon (EEUU); Dr. Richard D. Hurt (EEUU).
Idiomas oficiales: español, portugués e inglés
Programa científico: tendrá Unidades Temáticas que incluirán más de 250 conferencias a cargo de invitados especiales. Se desarrollarán simposios, ateneos, controversias, discusión de casos, cursos y presentación de trabajos de investigación.
Los participantes tendrán la posibilidad de acceder a audio y diapositivas de las sesiones más destacadas del CNC 2009, por ejemplo:
Más información: www.fac.org.ar/6cvc / 6cvc@fac.org.ar
VI Congreso Internacional de Cardiología por Internet
1ro. de Septiembre al 30 de Noviembre de 2009
Declarado de Interés Nacional
Res. Nº Res. Nº 363 - 361 - 04/2009
Presidencia de la Nación - Ministerio de Salud de la Nación Argentina.
Comienza hoy..
www.fac.org.ar/6cvc
Si aún no lo ha hecho, lo invitamos a inscribirse y a interactuar con los conferencistas y autores a través de los Foros de Discusión, donde los mensajes contarán con traducción.
Principales temas que se abordarán:
Cardiopatía Isquémica – RCP – Síndrome Metabólico – Dislipemias – Insuficiencia Cardíaca – Arritmias – Dispositivos electrónicos para el tratamiento de trastornos de la conducción – Enfermedad de Chagas – Hipertrofia ventricular – Investigación Clínica – HTA – Cirugía de revascularización – Angioplastia – Prótesis Endoluminales
Speakers internacionales que participarán en esta edición:
Dr. Paul A. Levine (EEUU); Dr. Adrian Baranchuk (EEUU); Dr. Andrés Ricardo Pérez Riera (Brasil); Dr. Jose Carlos Pachon (Brasil); Dr. Juan Carlos Chachques (Francia); Dr. Josep Brugada (España); Dr. Robert M. Lang (EEUU); Dr. Arturo Evangelista (España); Dr. Wilson Mathias (Brasil); Dr. James K. McCord (EEUU); Dr. Xavier Bosch (España); Dr. Michael A. Ross (EEUU); Dr. Juan José Badimon (EEUU); Dr. Richard D. Hurt (EEUU).
Idiomas oficiales: español, portugués e inglés
Programa científico: tendrá Unidades Temáticas que incluirán más de 250 conferencias a cargo de invitados especiales. Se desarrollarán simposios, ateneos, controversias, discusión de casos, cursos y presentación de trabajos de investigación.
Los participantes tendrán la posibilidad de acceder a audio y diapositivas de las sesiones más destacadas del CNC 2009, por ejemplo:
Más información: www.fac.org.ar/6cvc / 6cvc@fac.org.ar
Aug 30, 2009
How fast perfusion sequences help MO detection
A very interesting use of a rapid MR perfusion technique with high resolution (1.5x1.5) and full LV coverage.
Read the full text here in JCMR
Read the full text here in JCMR
Inflammation in Tako-Tsubo
An inflammatory disease after all?
Inflammation in takotsubo cardiomyopathy: insights from cardiovascular magnetic resonance imaging.
Eitel I, Lücke C, Grothoff M, Sareban M, Schuler G, Thiele H, Gutberlet M.
Read the abstract here
Inflammation in takotsubo cardiomyopathy: insights from cardiovascular magnetic resonance imaging.
Eitel I, Lücke C, Grothoff M, Sareban M, Schuler G, Thiele H, Gutberlet M.
Read the abstract here
Aug 27, 2009
Increasing Radiation in Medical Imaging - a window of opportunity for CMR

The recent NEJM manuscript on the increase in use of medical imaging modalities and radiation should be taken very seriously by payers, patients and practitioners. At the same time, the CMR community may be asking: should we care??? The definite answer is yes, because this issue is a big plus for CMR. We should emphasize this huge advantage of CMR and, again, educate cardiologists of the great risk/benefit ratio of the technique.
Aug 24, 2009
ESTAMOS ESTRATIFICANDO BIEN LOS PACIENTES CON CARDIOMIOPATIA HIPERTROFICA ?
Usefulness of cardiac magnetic resonance in assessing the risk of ventricular arrhythmias and sudden death in patients with hypertrophic cardiomyopathy
Sergio Leonardi1, Claudia Raineri1,*, Gaetano M. De Ferrari1, Stefano Ghio1, Laura Scelsi1, Michele Pasotti2, Marilena Tagliani2, Adele Valentini3, Roberto Dore3, Arturo Raisaro1 and Eloisa Arbustini2Aims: To assess the relationship between cardiovascular magnetic resonance (CMR) parameters and both spontaneous ventricular tachycardia (VT) and risk of sudden cardiac death (SCD) in hypertrophic cardiomyopathy (HCM) patients.
Methods and results: One hundred and eight consecutive HCM patients (mean age 42 ± 15 years, 76% males) underwent CMR evaluation and risk assessment. Delayed contrast enhancement (DCE) was quantified with a specifically designed score. Endpoints were either the presence of clinical VT/ventricular fibrillation (VF) or of acknowledged risk factors for SCD. Compared to patients without arrhythmia, those with VT/VF (n = 33) had a higher DCE score [median 8 (2–13) vs. 11 (6–20); P = 0.01]; DCE score was also the only independent predictor of VT/VF in the multivariable model. DCE score [median 6 (1–10.5) vs. 12 (6–18); P = 0.001], mean and maximal left ventricular (LV) wall thickness (MaxLVWT), as well as LV mass index were significantly greater among patients at risk for SCD (n = 51) compared with the remaining 57 patients at low risk. DCE score and MaxLVWT were independent predictors of SCD risk.
Conclusion: In HCM patients several CMR parameters are associated with risk for SCD. A semi-quantitative index of DCE is a significant multivariable predictor of both clinical VT/VF and of risk for SCD and may contribute to risk assessment in borderline or controversial cases.
Conclusion: In HCM patients several CMR parameters are associated with risk for SCD. A semi-quantitative index of DCE is a significant multivariable predictor of both clinical VT/VF and of risk for SCD and may contribute to risk assessment in borderline or controversial cases.
Key Words: Cardiovascular magnetic resonance • Sudden cardiac death • Hypertrophic cardiomyopathy • Ventricular tachycardia/fibrillation.
European Heart Journal 2009 30(16):2003-2010
Aug 23, 2009
It's education stupid!

Look at the results below: 80% of the responders think CMR will gain more use if cardiologists are more educated regarding how to use the tool. This is in great accordance to the results of the JACC paper providing the experience in Germany. We cannot stop reaching out to clinical cardiologists if we want CMR to overcome this underuse of the technique we see (at least in Brazil).
I personally do not know exactly how to do this but this is certainly the way to go.
Juliano
Look what CMR did in Germany!

CMR has had a great impact on German cardiology according to this article in JACC:
Read the abstract here
Aug 20, 2009
Electrocardiographic and cardiac magnetic
resonance imaging parameters as predictors
of a worse outcome in patients with
idiopathic dilated cardiomyopathy
Vinzenz Hombach1*, Nico Merkle1, Jan Torzewski1, Johann M. Kraus2,
Markus Kunze1, Oliver Zimmermann1, Hans A. Kestler2†, and Jochen Wo¨ hrle1†
Aims Clinical parameters are weak predictors of outcome in patients with idiopathic dilated cardiomyopathy (IDC). We assessed the prognostic value of cardiac magnetic resonance (CMR) parameters in addition to conventional clinical and electrocardiographic characteristics.
Methods and results One hundred and forty-one IDC patients were studied. QRS and QTc intervals were measured in 12-lead surface electrocardiogram. Patients were followed for median 1339 days, including 483 patient-years. The primaryendpoint—cardiac death or sudden death—occurred in 25 (18%) patients, including 16 patients with cardiac death, 3 patients with sudden cardiac death (SCD), and 6 patients with ICD shock. Late gadolinium enhancement (LGE) was detected in 36 patients (26%). Kaplan–Meier survival analysis displayed QRS .110 ms (P ¼ 0.010), the presence of LGE (P ¼ 0.037), and diabetes mellitus (P , 0.001) as significant parameters for a worse outcome. Multivariable analysis revealed cardiac index (P , 0.001), right ventricular end-diastolic volume index (RVEDVI) (P ¼ 0.006) derived from CMR imaging, the presence of diabetes mellitus (P ¼ 0.006), and QRS .110 ms (P ¼ 0.045) as significant predictors for the primary endpoint.
Conclusion Cardiac index and RVEDVI derived from CMR imaging in addition to QRS duration .110 ms from conventional surface ECG and diabetes mellitus provide prognostic impact for cardiac death and SCD in patients with IDC.
Keywords Idiopathic dilated cardiomyopathy † Magnetic resonance imaging † Late gadolinium enhancement † Prognosis
European Heart Journal (2009) 30, 2011–2018
Aug 17, 2009
Curso para atualizacao tecnica

O curso do ano passado foi muito bom. É um curso técnico, que reune basicamente especialistas onde se discutem assuntos raramente discutidos em outros eventos. Para quem faz os dois metodos, é uma oportunidade impar de discutirmos entre especialistas algumas duvidas comuns do dia-a-dia. Atualmente, é disparado o melhor evento para este fim.
Acesse o site aqui.
Subscribe to:
Posts (Atom)





